1 Primary open angle glaucoma
a. This is accounts for over 90% of all patients with glaucoma in the UK. This is caused by a failure of fluid inside the eye to escape from the eye at the trabecular meshwork.
2 Chronic angle closure glaucoma
a. This is more common in ‘long-sighted’ individuals who tend to have short eyes with a narrow angle between the iris and cornea.
3 Acute angle closure glaucoma
a. This is a speedier version of the above and causes a sudden, massive rise in intraocular pressure. The eye is very inflamed extremely painful. It may be preceded by haloes in the evening for a few days and is frequently accompanied by vomiting. Loss of vision can occur over 12 – 36 hours, so patients with these symptoms must get immediate attention from the eye casualty.
4 Normal tension glaucoma (low tension glaucoma)
a. This is caused by poor blood supply to the optic nerve. It is more difficult to detect, because the IOP is normal and can only confidently be diagnosed if progressive changes are observed in the optic disc or visual field. It is more common in women, especially those with a history of migraine.
5 Pigment dispersion glaucoma
a. This occurs whenthe iris is deeply set allowing the pigment behind it to rub on the zonules supporting the crystalline lens. Pigments gets rubbed off the back of the iris and deposits itself in the trabecular meshwork (located between the cornea and the iris), where fluid normally escapes from the eye.
b. This condition is usually first detected in young to middle aged short sighed men. If the IOP is not elevated, laser can create a small hole in the peripheral iris allowing the iris to lie in a more usual plane further forward in the eye.
6 Pseudoexfoliation glaucoma
This occurs because of the deposition of white flaky material onto the crystalline lens, pupil margin and most importantly the trabecular meshwork. It is often asymmetrical and can be a difficult glaucoma to treat.
7 Secondary glaucoma
a. There are many secondary forms of glaucoma, caused by trauma, bleeding, inflammation, previous surgery etc etc
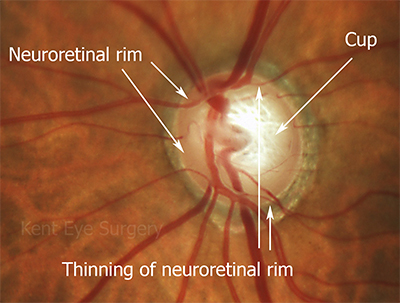
Damage to the optic disc
Nerve fibres transmitting visual information from the photoreceptors to the brain are lost in glaucoma resulting in characteristic changes on the surface of the optic nerve as it enters (or strictly leaves) the eye. Damage to the nerve fibres at the disk can be caused by raised eye pressure, reduce blood flow at the optic disc and possibly by reduced intracranial pressure (Ophthalmology June 2008). Ophthalmologists can examine your eye at the slit-lamp and often tell immediately whether or not you have glaucoma by the shape of the optic disc.
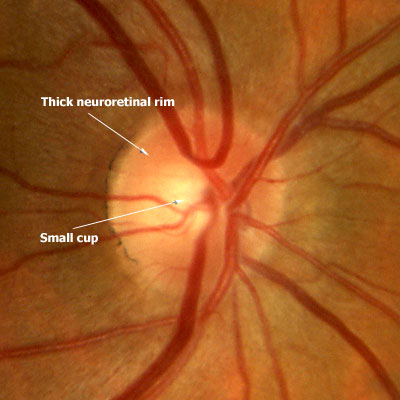
Compare a normal optic disc:
with an optic disc affected by glaucoma – the so-called cupped optic disc. Cupping means loss of neuroretinal rim tissue which means that the white bit or cup in the middle of the optic disc becomes larger.